Kaiser Permanente’s value-based, integrated care and coverage model differs from much of the United States health care system, which relies on disconnected clinical practices paid through fee-for-service. These disconnected approaches typically result in highly fragmented care, a focus on quantity of services with less focus on ensuring high-quality care, and an emphasis on acute care rather than long-term investments in population and community health.
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The challenge
Colorectal cancer is the third leading cause of cancer-related death and the third most common cancer in the United States.1 Colorectal cancer can affect anyone, but Black adults are disproportionately impacted compared to other groups. For example, compared to non-Hispanic whites, Black adults face higher rates of colorectal cancer incidence,2 younger age at diagnosis,3 later cancer stage at diagnosis,4 and worse stage-specific colorectal cancer mortality.5
Early detection dramatically improves outcomes. Precancerous growths (polyps) can be removed, and treatment is often highly successful when the cancer is identified early. The vast majority (91%) of people whose colorectal cancer is detected early survive at least 5 years, but only a little over a third (37%) of patients receive early diagnoses.6 If the cancer has spread to distant parts of the body, the 5-year survival rate is only 15%.7 Around 1 in 5 (22%) patients are diagnosed at this late stage.8
Colorectal cancer screening rates have increased, as the use of non-invasive, home-based screening methods like the FIT, or Fecal Immunochemical Test, have demonstrated their effectiveness and become more commonly used. Unfortunately, colorectal cancer screening rates remain lower than screening for other common cancers like breast and cervical cancer,9 and rates are lower among Black and Hispanic/ Latino adults than whites in the same age range.10 In many health systems, physicians do not actively reach out to patients to encourage colorectal cancer screening, but instead rely primarily on conversations with patients during medical office visits for other medical problems. Some adults of color face additional screening challenges related to health insurance coverage, access to physicians, stigma around colorectal screening, transportation access, ease of taking time away from work for screening appointments, or other factors.11
The integrated care and coverage solution
To increase colorectal cancer screening rates, Kaiser Permanente Northern California initiated an organized, population-based screening outreach program more than 15 years ago that continues today. The program mails FIT kits annually to members eligible for screening and offers on-request colonoscopy. Care teams reach out to members by mail, secure email, and telephone to encourage screening. In addition, while they are meeting with patients, physicians get an electronic health record reminder to encourage their patients to get screened.
Screening and outreach are designed to reach the full diversity of members. For example, the team conducted focus groups and used the findings to create targeted messages for outreach to Black and Hispanic/Latino members. Staff assess screening outcomes across racial and ethnic groups to track outreach effectiveness.
Members screened through the FIT who get a positive result, suggesting gastrointestinal bleeding, then get a colonoscopy to determine the cause of the bleeding. This is followed by further treatment and support as needed.
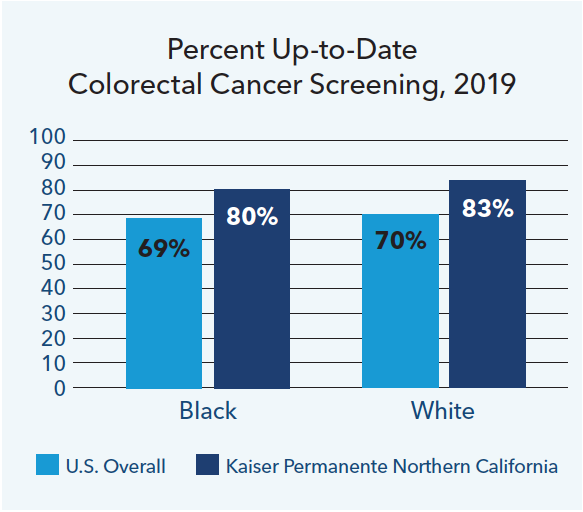
The percentages of members who were up to date on colorectal cancer screening doubled within a decade, resulting in higher screening rates than the national average.12 Similar screening and outreach approaches are being used throughout our organization, supported by discussions facilitated by Kaiser Permanente’s Care Management Institute and informal discussions between clinical leaders. Across Kaiser Permanente, we have achieved colorectal cancer screening rates for Black, white, Hispanic/Latino, and Asian members that are in the top 10% nationally. 13
How Kaiser Permanente’s integrated care and coverage model supported this innovation
Research and quality improvement
We analyze care management processes and outcomes and use the results to continuously improve. We then share findings from this practice-based clinical research to benefit others beyond Kaiser Permanente.
In our organization, research scientists, clinicians, medical groups, and health plan leaders collaborate to understand and improve colorectal cancer prevention and care. Over the last 15 years, Kaiser Permanente staff have published more than 550 journal articles on colorectal cancer, and these articles have been cited more than 23,000 times.14
Extensive population-level data
With access to data across large numbers of patients over long periods of time, Kaiser Permanente tracks population health trends, and identifies and pursues opportunities to improve and to eliminate disparities in care. Our extensive database and our research capacities allow us to serve as a helpful clinical and health services research partner to national agencies and academic institutions.
Our access to member data over long periods of time, because of low disenrollment rates, allows us to track patterns and understand implications. The Northern California colorectal cancer screening program, for example, tracked screening effectiveness for more than a decade. Results of the program were shared in the New England Journal of Medicine,15 so other health care organizations and health care teams could learn from our experiences.
Our research studies influence medical practice, within and beyond Kaiser Permanente. For example, a study by Kaiser Permanente researchers on the effectiveness of FIT was cited in screening recommendations by the U.S. Preventive Services Task Force.16 The task force makes evidence-based recommendations on best practices in clinical preventive services that are used by clinicians and health care organizations across the country. Kaiser Permanente studies also helped establish criteria for colonoscopy quality, which increases effectiveness of colorectal cancer screening.17
Focus on individual and population health
Our mission, and our long-term perspective — free from investors’ focus on short-term returns — motivates us to address individual and community drivers of health. We analyze member health trends to identify opportunities for improvement, support quality improvement and prevention, and eliminate racial and economic disparities.
Kaiser Permanente is committed to ensuring equitable access to high-quality care across the care continuum, from prevention and screening through treatment and post-treatment care. Articles in peer-reviewed journals have described how Kaiser Permanente’s integrated, equity-focused approach has reduced or even eliminated racial disparities in screening and care. In addition to colorectal cancer screening, we eliminated disparities in mortality and medication adherence rates among Black and Latino HIV-positive patients,18 and we nearly eliminated disparities for cardiac risks and diabetes markers between Black and white seniors, in contrast to other health plans in the western United States.19
The colorectal cancer screening program materials and outreach focused on reaching the full diversity of our members, and we continue working to improve our outreach. Measuring our progress allows us to continually assess outcomes and make improvements to ensure that everyone has the best possible health care and health outcomes.
Connected, coordinated care teams
Members benefit from well-coordinated care in the Kaiser Permanente system. Clinicians can easily coordinate with one another and seamlessly refer patients to other team members — primary care doctors, specialists, lab technicians, pharmacists, and other health care professionals.
In the colorectal cancer screening program, care team members identify who is at highest risk and coordinate outreach by mail, secure email, and phone. Centralized tracking allows us to monitor screening and follow up with members to maximize participation rates. Physicians are supported through automated electronic medical record reminders to conduct direct, in-person outreach to their eligible patients. Patients mail their FIT kits directly to Kaiser Permanente labs, through pre-addressed mailers with pre-paid postage, and then lab staff determine test results and securely share the results with physicians and their patients.
If test results are positive, staff work with the patient to schedule a colonoscopy, conducted by a gastroenterologist. When cancer is found, oncologists and team members develop a treatment plan with the patient and provide ongoing support. Coordination across this network of care team members, through every step of the process, improves screening rates, helps us identify cancer early, and supports timely treatment.
