Medicaid provides health coverage to eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. Medicaid is administered by states, according to federal requirements and is jointly funded by states and the federal government. Hawaii’s Medicaid program is known as QUEST Integration (Quality care, Universal access, Efficient utilization, Stabilizing costs, Transforming the way health care is provided)
Enrollment
More than 47,000 Kaiser Permanente members are enrolled in QUEST (Medicaid) in Hawaii. 39% are children, 56% are adults, and 5% are seniors.

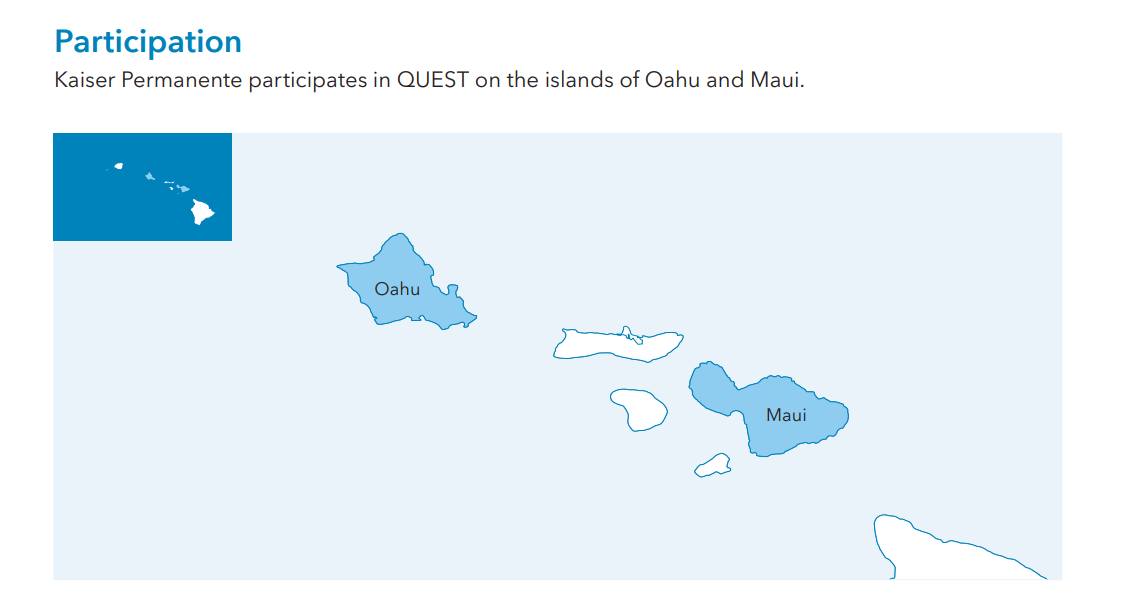
Areas Served
Kaiser Permanente contracts directly with the state to provide care and coverage on a capitated basis (meaning a fixed payment per member, per month) and has managed long-term services and supports for our QUEST members since 2015. Kaiser Permanente also serves people who are dually eligible for Medicare and Medicaid through a Fully Integrated Dual Eligible Special Needs Plan (DSNP). Children in Hawaii can receive continuous coverage until their sixth birthday, and from ages 6-19 receive coverage for 2 years at a time
State Program Spotlight
Kaiser Permanente provides several Medicaid benefits that help address social needs and improve outcomes for our members, especially those with the most complex needs.
The Health Coordination Services Program is a key benefit for members with Special Health Care Needs, Expanded Health Care Needs, and members receiving Long Term Services and Supports.
Special Health Care Needs (SHCN) – Adults and children with SHCNs are members that have chronic physical, behavioral, developmental, or emotional conditions that require health-related services of a type or amount that is beyond what is required of someone of their general age.
Expanded Health Care Needs (EHCN) – A member with EHCN has complex, costly health care needs and conditions, or whose risk of developing these conditions is imminent. EHCN services are provided to adults and children that meet the qualifications of the EHCN population due to the member having met one or more medical conditions, such as serious mental illness, substance use disorder, or chronic health condition.
Long Term Services and Supports (LTSS) – LTSS populations includes members in an inpatient medical facility receiving Nursing Facility Level of Care. These facilities include assisted living facilities, expanded adult care homes, community care foster family homes, nursing facilities, and sub-acute units.
Going Home Plus (GHP) and Institutional Relocation Services — Person-centered relocation services are provided to help members in institutions (i.e., hospitals, psychiatric residential treatment facilities, prisons, nursing homes, or other long-term care facilities). This population may include youth with mental illness; the elderly; or individuals who have physical, intellectual, and developmental disabilities. GHP helps them to move out and receive services to live in their own homes and communities.
Community Integration Services (CIS) – CIS provides pre-tenancy and tenancy sustaining services that support individuals to be prepared and successful tenants in housing that is owned, rented, or leased to the individual. Pre-tenancy supports help to identify the individual’s needs and preferences, assist in the housing search process, and help to arrange details of the move. Tenancy sustaining services help with independent living sustainability that includes tenant/landlord education, and tenant coaching and assistance with community integration and inclusion to help develop natural support networks. Services are provided by CIS providers and our clinical and non-clinical staff, including health coordinators and community health workers.
Quality
Since 2017, the National Committee for Quality Assurance (NCQA®) has awarded Kaiser Permanente’s QUEST plan 4.5 out of 5 stars for our performance on measures related to consumer satisfaction, prevention, and treatment. Kaiser Permanente QUEST performs above the National Committee for Quality Assurance (NCQA®) 90th percentile** for the following measures:
- Immunization for Adolescents Combo 2
- Colorectal Cancer Screening
- Asthma Medication Ratio
- Controlling High Blood Pressure
- Eye Exam for Patients with Diabetes
These metrics are based on NCQA’s Healthcare Effectiveness Data and Information Set (HEDIS), a tool used by more than 90% of America’s health plans to measure performance on important dimensions of care and service. **Measures reflect Kaiser Permanente QUEST performance among all Medicaid plans nationally in 2023
Social Health
Many Kaiser Permanente members struggle with inadequate housing, hunger, financial stress, and other circumstances that create barriers to good health, particularly members enrolled in Medicaid. Kaiser Permanente works proactively to identify our members with these and other adverse social needs and to connect them to community-based programs and government assistance-programs that can support their well-being.
Safety-Net Partnerships
Kaiser Permanente is committed to building partnerships with the health care “safety net” — institutions that play a critical role in delivering health care for the uninsured and underserved. Through grants, training, and technical assistance, we work with safety-net hospitals and health centers to help these institutions reach those who are low-income, uninsured, or under-resourced in our communities, and move the needle in eliminating health disparities. We do this by investing in quality improvement and other support efforts that aim to transform care and improve health access for those most in need.
Social Health Screening and Identification
Kaiser Permanente uses standard social health screening questions and data analytics to identify members vulnerable to food-insecurity, homelessness, financial strain, and other adverse social factors. By expanding social health screenings across an increasing number of clinical settings and member service touchpoints, with a focus on high-risk populations, Kaiser Permanente is steadily increasing the number of members screened for social needs every year. We screened nearly 3 million members for social needs in 2024, including 32% of our Medicaid members. These screenings and other data sources helped us identify over 1 million members with social needs and connect nearly 500,000 members to public benefits and community-based programs that support overall health.
The Kaiser Permanente Community Support Hub™
The Kaiser Permanente Community Support Hub™ is dedicated to helping people meet their basic needs. The Hub operates proactively, using text, email, and phone calls to encourage members to complete social health screenings and to offer help finding and enrolling in community-based resources and government assistance programs that support overall health. The Hub also provides on-demand services, including an online directory of resources that anyone can use to search for local programs that help with housing, food, paying utility bills, and more.
Medical Legal Partnerships
Working with local legal aid organizations in our communities, our care teams help patients facing housing-insecurity receive legal help at no cost. These medical-legal partnership programs build the capacity of the legal services sector and increase access to legal services to prevent people and families from losing their homes. This program targets low-income members and patients with housing related legal needs. In 2024, legal consultation was provided to over 1,000 patients across our national footprint.
