
Integrated Care Stories
Reducing hip fracture rates in at-risk patients
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The challenge
Each year in the United States, around 300,000 seniors are hospitalized for hip fractures.1 The consequences of these fractures can be severe. Osteoporosis related bone fractures lead to more hospitalizations than heart attack, strokes, and breast cancers combined.2 Hip fractures double the risk of mortality and quadruple the risk that a patient will need long-term nursing facility care.3 Yet throughout the country, few seniors receive preventive care that could reduce their fracture risk. Even after a fracture occurs, few patients are given bone scans or offered bone-protecting drugs.4
The integrated care and coverage solution
A small team of Kaiser Permanente clinicians in Southern California designed an approach that they hoped would reduce the number of fractures they were seeing in their clinics. They reviewed Kaiser Permanente data, set a fracture reduction target, and created a plan to identify at-risk patients. Once identified, staff members reached out to these patients to ensure they got a bone density scan and were receiving any needed treatments. The team assessed their approach and outcomes and made changes to maximize the effectiveness of the program.
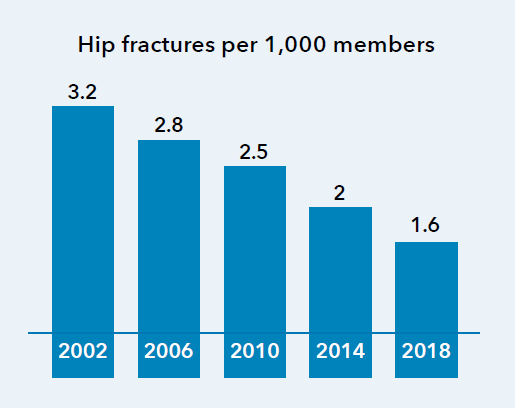
The Healthy Bones Program reduced hip fracture rates by around 50% between 2002 and 2018, as seen in the chart.5
How Kaiser Permanente’s integrated care and coverage model supported this innovation
High-quality care with clinical decisions made by doctors and patients
Physicians work with their patients to develop personalized care plans, making decisions about medical care together. To inform those decisions, doctors use the best available evidence and create clinical practice guidelines. They champion quality improvement, ensuring that our care teams practice medicine based on the best, most up-to-date information, incorporating innovative approaches.
Clinicians collaborated to design, launch, and oversee a process to analyze data and then develop and implement a program to reduce fracture rates.
“In other countries, and within some medical networks … including the Kaiser Permanente system … there are coordinated services to assure appropriate post-fracture follow-up. In 2013, the International Osteoporosis Foundation introduced a campaign … to assure that ‘fragility fracture sufferers receive appropriate assessment and intervention to reduce future fracture risk,’ but such organized preventive measures have remained rare in the United States.”
— Jane Brody, The New York Times
Flexibility within a budget
The Kaiser Foundation Health Plan collects member premiums in advance and then pays delivery system partners for members’ care throughout the year. This creates the flexibility within and across the health plan, the hospitals, and the medical groups to deploy those resources to best meet our members’ needs. Instead of relying on revenues generated when patients are sick, we are incentivized to invest in longer-term infrastructure and population health investments that improve long-term outcomes, and to provide timely, effective, and efficient care and service.
Leadership recognized the potential to improve care and reduce costs, and supported physician-led efforts to reduce fracture rates by providing time, infrastructure, analytics, funding, and other supports.
Research and quality improvement
With access to data across large numbers of patients over long periods of time, Kaiser Permanente tracks population health trends, and identifies and pursues opportunities to improve and to eliminate disparities in care. We analyze care management processes and outcomes and use the results to continuously improve.
Using data on fracture trends across the Kaiser Permanente patient pool, physicians identify which patients are most at risk for fractures and then care teams follow up with these patients to ensure they are getting bone scans and needed care. Kaiser Permanente tracks care quality, outcomes, and process metrics to ensure the program is working as intended.
Connected, coordinated care teams
Clinicians can easily coordinate with one another and seamlessly refer patients to other team members — primary care doctors, specialists, lab technicians, pharmacists, and other health care professionals.
Care team members contact at-risk Kaiser Permanente members to ensure they get bone density scans and needed treatment, and clinicians handle patient visits, scans, and follow-up.
Focus on individual and population health
Kaiser Permanente’s mission is to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. This mission, and our long-term perspective motivates us to address individual and community drivers of health. Investments in individual and population health help us retain our members, and we benefit when those long-tenured members and the broader communities we serve realize positive health outcomes.
Reducing fracture rates helps our patients stay healthy. This has reduced fracture-related hospitalizations and mortality rates.
Kaiser Permanente’s integrated care and coverage model differs from much of the United States health care system, which relies on disconnected clinical practices paid through fee-for-service. These disconnected approaches typically result in highly fragmented care, a focus on quantity of services rather than high-quality care, and an emphasis on acute care rather than long-term investments in population and community health.
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
After a Broken Bone, the Risk of a Second Fracture
Far too few patients are referred for treatment that could stave off another costly, debilitating and sometimes deadly fracture.
1 National Center for Injury Prevention and Control at the Centers for Disease Control and Prevention, Hip Fractures Among Older Adults, https://www.cdc.gov/homeandrecreationalsafety/falls/adulthipfx.html, accessed February 2, 2021.
2 Dane Hansen, FSA, MAAA, Carol Bazell, MD, MPH, Pamela Pelizzari, MPH, Bruce Pyenson, FSA, MAAA, “Medical Cost of Osteoporotic Fractures,” Milliman Research Report, August 2019.
3 Gabriel S. Tajeu, et al., “Death, Debility, and Destitution Following Hip Fracture,” The Journals of Gerontology Series A, Biological Sciences and Medical Sciences, March 2014, p. 346.
4 Jane E. Brody, “After a Broken Bone, the Risk of a Second Fracture,” The New York Times, November 9, 2020, Section D, p. 7.
5 Analysis of Integrated Data Repository data for patients age 60 and above, maintained by Kaiser Permanente Insight, provided by Navraj Mudahar, MHA, and Grace Xuan Chen, PhD, Kaiser Permanente Southern California, February 2021.