The United States is facing a mental health crisis that requires new and innovative approaches to mental health care including tele-behavioral health.. Even prior to the pandemic, mental health challenges were the leading cause of disability and poor life outcomes in young people, with up to 1 in 5 children ages 3 to 17 with a reported mental, emotional, developmental, or behavioral disorder. In 2023, roughly 3 in 10 adults reported symptoms of depression or anxiety disorder and 1 in 10 youth reported experiencing depression that severely impaired their ability to function at school or work, at home, with family, or in their social life.
During the pandemic, tele-behavioral health services played a critical role in increasing access to care while staying safe at home. In response to demand, health care systems developed new telehealth services or expanded existing virtual offerings, often increasing their investments in infrastructure. Many faced multiple barriers, including high startup costs, outdated equipment, lack of provider buy-in, workflow challenges, and user issues. Through this process, the entire system of care became more robust and dynamic. Today, telehealth continues to be attractive option for mental health services despite a widespread return to other in-person activities in health care settings.
Our approach to providing tele-behavioral care
When it comes to providing tele-behavioral health care, Kaiser Permanente supports prevention, early intervention, and treatment for emotional health and wellness with a variety of evidenced-based digital tools, including video and telephone appointments and therapeutics. In this context, the term “tele-behavioral health” means the use of phone and video technology, along with supportive digital services, to provide care for people with a wide range of mental health conditions.
Patients can enter our system through a variety of avenues, including self-referral, referral from primary care into Collaborative Care, clinician referral to a specialty provider, or taking an assessment (such as a PHQ-9 or GAD-7) supported by clinician-guided navigation. A clinician can also guide members to a suite of digital resources within our system, some of which are open to all members and others which require a referral.
Everyone is on a different journey when it comes to mental health, so our suite of digital options reflects the varying needs, lifestyles, and learning styles of our members. Our digital tools are piloted in clinical settings and reviewed to ensure a quality user experience, a strong evidence-base, and alignment with our organization’s commitment to equity, inclusion, and diversity. These resources include user-friendly, educational resources, such as articles, videos, and podcasts, along with a variety of mental health applications. Several digital therapeutic applications are available at no cost to members directly from kp.org.
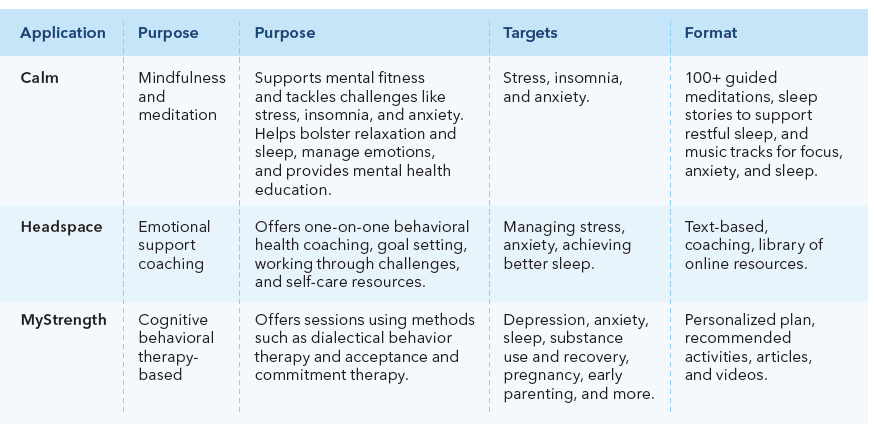
This year, we expanded the suite of digital therapeutics available for clinician referral to meet additional member needs. For example, new resources will support women during pregnancy and post-partum, cancer patients, parents, and youth ages 13 and older who are coping with depression, anxiety, and self-harm. Clinicians find that having these tools integrated into care delivery, and easily accessible, expands and modernizes the capabilities of their practice. Early qualitative data suggest that these tools can provide significant help for patients with mild to moderate anxiety, depression, and other mental health issues.
Policy opportunities to support tele-behavioral health
At Kaiser Permanente, we believe everyone should have access to high quality, evidence-based behavioral health services, integrated with their medical services. Telehealth capabilities and digital therapeutics are powerful tools in supporting mental health, and policymakers are actively seeking ways to ease and expand pathways to care. Public policy opportunities abound when it comes to supporting mental health care through different telehealth modalities, inclusive of phone, video, and digital applications. Critical among them include:
- Supporting states in developing and adopting interstate compacts for mental health professionals,
- establishing adequate reimbursement mechanisms,
- ensuring patient privacy and data security,
- supporting technology adoption and infrastructure development,
- promoting training and education for mental health professionals, and
- enforcing quality assurance standards
To ensure that every person can reap the benefits of telehealth, successful policies should address barriers like internet connectivity and technology affordability. Advancing these policies will expand
access to mental health services, enhance the quality of care, and ensure equitable delivery of telehealth services across diverse populations.
