
Integrated Care Stories
Hepatitis C Care Cascade
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The challenge
Prior to the COVID-19 pandemic, the hepatitis C virus, or HCV, killed more people in this country than any other infectious disease.1 HCV frequently has few noticeable symptoms and can eventually cause hepatitis C, a liver infection. When symptoms finally appear, they often indicate advanced liver disease. The rate of new HCV infections has more than doubled in recent years.2
HCV spreads through contact with an infected person’s blood. HCV infection can occur many different ways, including getting tattoos or body piercings using unsterile equipment, sharing injection drug equipment, or having received a blood transfusion before 1992 when blood supplies started being screened for the virus. Because people can have HCV for years without symptoms, they may unknowingly transmit HCV to others. Most patients do not know how they contracted HCV.
In the 1990s, drug companies discovered HCV treatments, but the drugs were not effective for many people and often caused serious side effects.3 Then from 2014 through 2017, new treatments were approved that could achieve high cure rates with minimal side effects. Around the same time, the U.S. Preventive Services Task Force began recommending screening for baby boomers — considered at higher risk for HCV — and this recommendation was later expanded to include all adults age 18 through 79.
Now, tests detect the virus and treatment can eliminate most HCV infections in 8 to 12 weeks. Left untreated, though, HCV can cause liver damage, cirrhosis, liver cancer, and even death.4
The integrated care and coverage solution
In our Mid-Atlantic Region (Washington, D.C., and parts of Maryland, and Virginia), Kaiser Permanente developed a new process to screen at-risk patients for HCV, building on existing research. In the first step of the Hepatitis C Care Cascade, care teams identify patients prioritized for HCV testing through our secure electronic health record system and then reach out to offer testing. Baby boomers were initially prioritized for testing, and this was later expanded to include all adults age 18 to 79 per U.S. Preventive Services Task Force recommendations.
When patients have a medical visit, an electronic health record alert notifies the care team of preventive screenings that are due, including the HCV test. The alert provides sample language for discussing the benefits of screening and patients are given written information about the test. Once patients agree to screening, their physican places an order authorizing the complete pathway of HCV tests and related diagnostic tests that may be needed. The HCV test is conducted the next time patients go to the lab for various preventive screening tests. HCV testing only requires a single trip, since the lab collects enough blood for the 2 tests needed to diagnose HCV.
When the tests indicate HCV infection, a care coordinator connects the patient to a gastroenterologist so the patient can learn more about their diagnosis and get medication to cure the virus. Additional tests determine whether HCV has caused liver damage and additional support is needed. A care coordinator updates patients throughout the process and provides reassurance and resources at every step.5
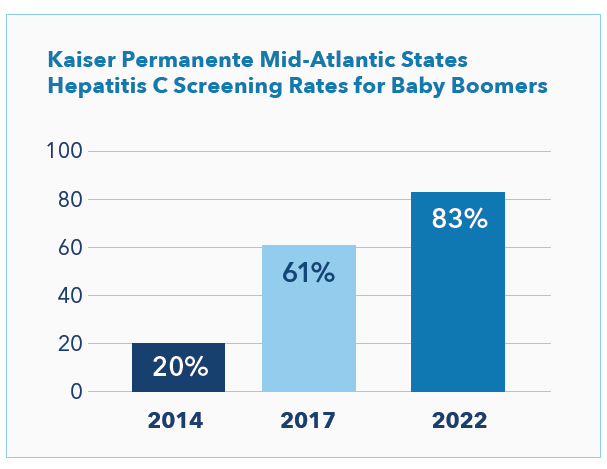
Since implementation of the Hepatitis C Care Cascade, the percentage of baby boomers screened has grown from 20% to 83% (see chart), and the percentage of people age 18 to 79 screened is now 67%.6 These rates are likely much higher than typical. For comparison, the 2017 National Health Interview Survey data found that only 17% of the surveyed baby boomer population responded “yes” when asked if they had ever had a blood test for hepatitis C.7 Kaiser Permanente’s Hepatitis C Care Cascade program had achieved a 61% screening rate at that time (see chart), calculated based on Kaiser Permanente’s screening records and completion of the full care cascade rather than a single blood test.8
How Kaiser Permanente’s integrated care and coverage model supported this innovation
Focus on individual and population health
Our mission and our long-term perspective – free from investors’ motivates us to address individual and community drivers of health. We analyze member health trends to identify opportunities for improvement and support quality improvement and prevention. These investments in individual and population health help us retain our members, and Kaiser Permanente benefits when those long-tenured members and the broader communities we serve realize positive health outcomes.
We focus on early detection to prevent or reduce the long-term effects of the virus. By encouraging patients to get screened and providing a streamlined screening process, we achieve higher screening rates than typical, and can provide earlier treatment. Timely treatment reduces the risk of liver failure and the need for liver transplants due to advanced disease. In addition to the benefits for individual members, HCV is an infectious disease that can be unknowingly transmitted to others — so our communities also benefit from increased outreach and treatment.
Flexibility within a budget
The Kaiser Foundation Health Plan collects member premiums in advance and then pays care delivery system partners for members’ care throughout the year. Instead of relying on revenues generated when patients are sick, we are incentivized to invest in longer-term infrastructure and population health investments that improve long-term outcomes, and to provide timely, effective, and efficient care and service that allows us to retain and expand our membership.
Drugs to cure HCV are very expensive. Some studies suggest that curing HCV can ultimately reduce costs over many years, which only incentivizes investment in prevention when people stay with their health plans over many years.9 We retain members for a long time, so early treatment allows us to avoid the future costs of treatment for long-term members whose HCV infection would have caused serious illness.
Nonetheless, like other health systems, we pay extraordinarily high prices for the drug. We are committed to supporting the long-term individual and population health outcomes of our members, so we invest in HCV screening and early treatment even though many people who are infected might never progress to advanced disease. We are advocating for more reasonable and fair drug pricing for HCV drugs as well as other high-priced drugs, for the benefit of our members, the communities we serve, and the overall health system.
Connected, coordinated care teams
Clinicians can easily coordinate with one another and seamlessly refer patients to other team members — primary care doctors, specialists, lab technicians, pharmacists, and other health care professionals.
The Hepatitis C Care Cascade process streamlines a complex testing protocol and improves testing rates through effective coordination. For example, by eliminating the need for a second lab visit to confirm HCV diagnosis we reduce the risk that some patients might not complete it.
Multiple team members provide support. Clinicians discuss options with their patients and order and analyze tests. Depending on the outcome of the tests, patients may receive treatment and continued monitoring from an infectious disease specialist, a gastroenterologist, or their primary care physician. A care coordinator walks the patient through the care cascade, tracks tests, answers 4 questions, schedules follow-up visits, and ensures that their physicians are informed throughout the process. Care team members can access patients’ full range of relevant medical information to ensure coordinated care.
Research and quality improvement
We analyze care management processes and outcomes and use the results to continuously improve. We then share findings from this practice-based clinical research to benefit others beyond Kaiser Permanente. In addition, our care teams can access a constantly updated clinical library, helping us stay abreast of additional new evidence-based approaches.
The Hepatitis C Care Cascade toolkit has been shared with colleagues across Kaiser Permanente, inspiring others to adopt similar lab testing and care coordination strategies. All Kaiser Permanente health care teams benefit from easy access to data and coordination across care team members.
We also have shared information about the program with experts at the Centers for Disease Control and Prevention and the National Institutes of Health and with others in the field through publications and scientific conferences. The Hepatitis C Care Cascade approach has been commended by the World Health Organization as an innovation in hepatitis care. 10
Kaiser Permanente’s integrated care and coverage model differs from much of the United States health care system, which relies on disconnected clinical practices paid through fee-for-service. These disconnected approaches typically result in highly fragmented care, a focus on quantity of services rather than high-quality care, and an emphasis on acute care rather than long-term investments in population and community health.
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
Hepatitis C treatment
Learn more about diagnosis and treatment at Kaiser Permanente.
1. Howard, Jacqueline. “Rate of New US Hepatitis C Infections Rises Threefold in the Past Decade, New Report Finds.” CNN, Cable News Network, 10 Apr. 2020, https://edition.cnn.com/2020/04/10/health/hepatitis-c-infection-rate-rises/index.html.
2. “2020 Viral Hepatitis Surveillance Report.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, United States, 2020, https://www.cdc.gov/hepatitis/statistics/2020surveillance/index.htm. Published September 2022.
3. “Then and Now: The Evolution of Treatments for Hepatitis C.” Healthline, 9 March 2018, https://www.healthline.com/health/hepatitis-c/evolution-of-treatments#the-future.
4. “What Is Hepatitis C – FAQ.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 28 July 2020, https://www.cdc.gov/hepatitis/hcv/cfaq.htm#:~:text=Hepatitis%20C%20can%20be%20a,liver%20cancer%2C%20and%20even%20death.
5. Jonas, M. Cabell, et al. “Streamlining Screening to Treatment: The Hepatitis C Cascade of Care at Kaiser Permanente Mid-Atlantic States.” OUP Academic, Oxford University Press, 16 Feb. 2016, https://academic.oup.com/cid/article/62/10/1290/2462676.
6. Data provided by Dr. Cabell Jonas, Director of Research Programs and Research Scientist, Mid-Atlantic Permanente Research Institute from internal research dashboard on May 25, 2022.
7. Patel, Eshan U et al. “Limited Coverage of Hepatitis C Virus Testing in the United States, 2013-2017.” Clinical infectious diseases : an official publication of the Infectious Diseases Society of America vol. 68,8 (2019): 1402-1405. doi:10.1093/cid/ciy803
8. Kaiser Permanente data provided by Dr. Cabell Jonas, Director of Research Programs and Research Scientist, Mid-Atlantic Permanente Research Institute from internal research dashboard on May 25, 2022; Rodriguez-Watson, Carla et al. “Hepatitis C Care Pathway Associated With Increased Screening, Confirmation, and Diagnosis Communication to Patients.” Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association. Vol. 19,3 (2021): 607-609.e2. doi:10.1016/j.cgh.2019.12.038
9. Padula, J, et al. “Cost-Effectiveness of Total State Coverage for Hepatitis C Medications.” The American Journal of Managed Care, May 20, 2021, https://www.ajmc.com/view/cost-effectiveness-of-total-state-coverage-for-hepatitis-c-medications. Rattay, T, et al. “Cost-Effectiveness of Access Expansion to Treatment of Hepatitis C Virus Infection Through Primary Care Providers.” Gastroenterology, October 23, 2017, https://www.gastrojournal.org/article/S0016-5085(17)36275-3/fulltext#secsectitle0040. Linas, BP and Nolen, S. “A Guide to the Economics of HCV Cure in 2017.” Infectious Disease Clinics of North America, June 2018, 32(2), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6085105/.
10. Tucker, Joseph, et al. “The HepTestContest: A Global Innovation Contest for Identify Approaches to Hepatitis B and C Testing.” BMC Infectious Diseases, November 1, 2017, https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-017-2771-4.