
The nation is facing a shortage of mental health workers, and public policy is needed to address the challenge
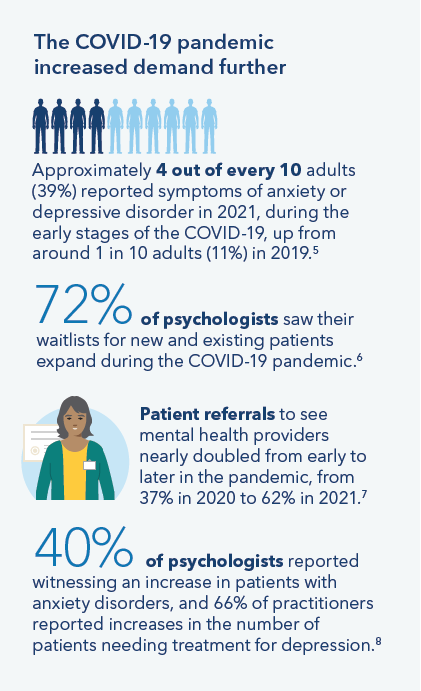
The COVID-19 pandemic highlighted structural challenges facing America’s health care system, especially employee shortages and a lack of racial and ethnic diversity and linguistic capabilities. While these challenges existed prior to the pandemic, they intensified during the global health emergency and are expected to grow significantly if unaddressed.

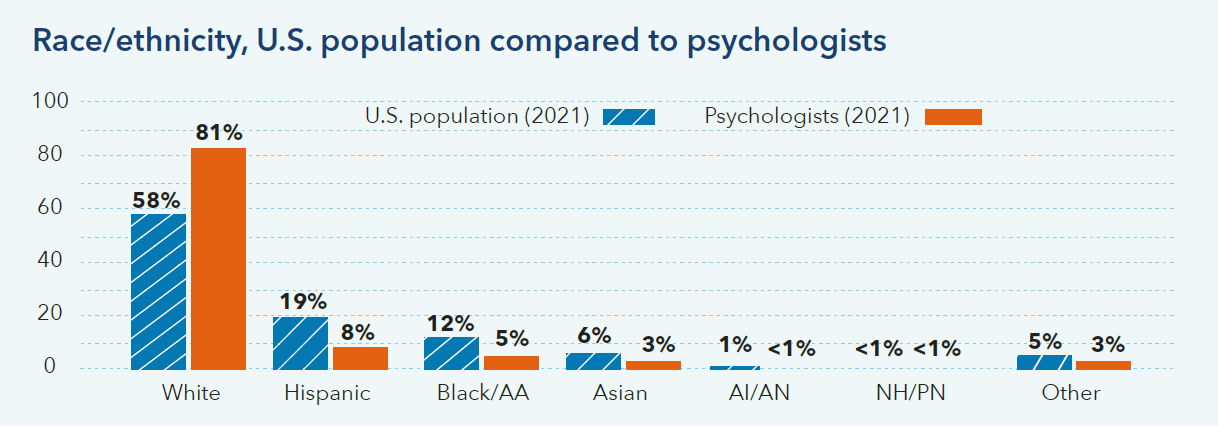
The mental health workforce is less diverse than the populations they serve
For example, nationally, psychologists are less diverse than the U.S. population.2
Public Policy
To address the problem, Kaiser Permanente is focusing on hiring and retention of mental health workers and launching new programs to expand and diversify the workforce. These are important steps, but public policy also is needed to address the challenge at scale across the country. Kaiser Permanente supports several approaches:
- Conduct and share additional research on workforce trends. The U.S. Health Resources and Services Administration (HRSA) should reevaluate the current and future adequacy of the behavioral health workforce, considering trends in demand/utilization and changing modes of practice, such as telehealth. In addition, HRSA should evaluate mental health
- Increase funding for residency and other mental health physician training programs. Federal policymakers should expand and restructure federal Graduate Medical Education funding to increase the number of psychiatry, addiction medicine, and child psychiatry residency positions and fellowships and establish new residency programs. In addition, states and hospitals should be incentivized to contribute matching funds for new residency programs.
- Support programs to expand and diversify the behavioral health workforce and make care easier to access. Institutions and policy leaders should invest in programs to diversify the behavioral health workforce and increase the number of practitioners trained to deliver services to medically underserved populations, including people of color. Leaders also should support state curriculum development, specialized training, and certification of behavioral health peers and community health workers, and promote team-based approaches that can make behavioral health services easier to access.
- Streamline training requirements to minimize economic burden and enable more people from diverse backgrounds to enter the mental/behavioral health professions. Policymakers should promote expanded, well-designed education, training, and fellowship opportunities that reduce the total cost of attaining degrees and licensure, with particular focus on support and mentorship for diverse mental health practitioners.
- Promote the use of telehealth and technology to improve access and enable more flexible care and scheduling. More states should adopt state licensing compacts, which allow mental health practitioners to provide care to patients in states that have joined the compact.
References
- Weiner, Stacy, “A Growing Psychiatrist Shortage and an Enormous Demand for Mental Health Services,” AAMC News, August 9, 2022, https://www.aamc.org/news-insights/growing-psychiatrist-shortage-enormous-demand-mental-health-services#:~:text=Already%2C%20more%20than%20150%20million,overextended%20as%20well%2C%20experts%20say.
- American Psychological Association Center for Workforce Studies, “Data Tool: Demographics of the U.S. Psychology Workforce (Interactive Data Tool),” retrieved February 10, 2023, https://www.apa.org/workforce/data-tools/demographics; and Kaiser Family Foundation, “Population Distribution by Race/Ethnicity, 2021,” State Health Facts, https://www.kff.org/other/state-indicator/distribution-by-raceethnicity/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
- Health Workforce Division of the Health Resources and Services Administration, U.S. Department of Health and Human Services, “Behavioral Health Workforce Projections, 2017-2030,” https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/bh-workforce-projections-fact-sheet.pdf.
- Bureau of Health Workforce, Health Resources and Services Administration, U.S. Department of Health and Human Services, “National Projections of Supply and Demand for Selected Behavioral Health Practitioners, 2013-2025,” November 2016, https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/behavioral-health-2013-2025.pdf.
- Panchal Nirmita, et al, “The Implications of COVID-19 for Mental Health and Substance Abuse,” KFF, March 20, 2023, https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/.
- National Center for Health Statistics, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, “Estimates of Mental Health Symptomatology, by Month of Interview, United States, 2019,” National Health Interview Survey, March 2021, https://www.cdc.gov/nchs/data/nhis/mental-health-monthly-508.pdf.
- American Psychological Association, “Increased Need for Mental Health Care Strains Capacity,” November 15, 2022, https://www.apa.org/news/press/releases/2022/11/mental-health-care-strains.
- American Psychological Association, “Demand for Mental Health Continues to Increase,” October 19, 2021, https://www.apa.org/news/press/releases/2021/10/mental-health-treatment-demand/.
- American Psychological Association, “Increased Need for Mental Health Care Strains Capacity,” November 15, 2022, https://www.apa.org/news/press/releases/2022/11/mental-health-care-strains.