
Integrated Care Stories
Enhanced recovery after surgery
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The challenge
Around 25% of all surgery patients across the nation suffer postoperative complications.1 These can lead to serious health problems and even death, and can increase health care costs. To help address the problem, health care leaders in northern Europe developed Enhanced Recovery After Surgery ERAS programs — a team-based approach used before, during, and after surgery to reduce complications. Some health care teams in additional countries, including the United States, began using ERAS programs over the last 2 decades.2
Surgery protocols have long assumed patients should fast the morning before surgery, receive opioids to control pain, and rest in bed to recover.3 In contrast, ERAS programs reduce fasting before anesthesia, increase use of non-opioid pain relievers and reduce opioid use, encourage people to more quickly return to normal diet and activities, and offer more extensive patient education.
Researchers have tested ERAS programs and found they clearly shorten hospital stays. But with few opportunities to test ERAS in large-scale, real-world settings, it has been challenging to evaluate different ERAS approaches or consistently achieve reductions in complications such as cardiac, pulmonary, and neurologic problems.4
The integrated care and coverage solution
A Kaiser Permanente team in Northern California decided it would try to reduce postoperative complications through an ERAS program. The team developed an ERAS protocol for use in a large-scale, real-world setting to identify approaches that reduce complication rates.
Instead of asking patients to fast before surgery, the care team would encourage patients to eat food 8-12 hours before surgery and give them a high-carbohydrate drink a few hours before surgery. They would provide additional nutrition within 12 hours after surgery. The team would give patients non-opioid pain-relievers, encourage patients to begin walking within 12 hours of surgery, and help them set and maintain daily walking goals. They also would strive to lessen patients’ anxiety by providing a clear roadmap of surgical and recovery activities and encouraging them to participate actively in their recovery.
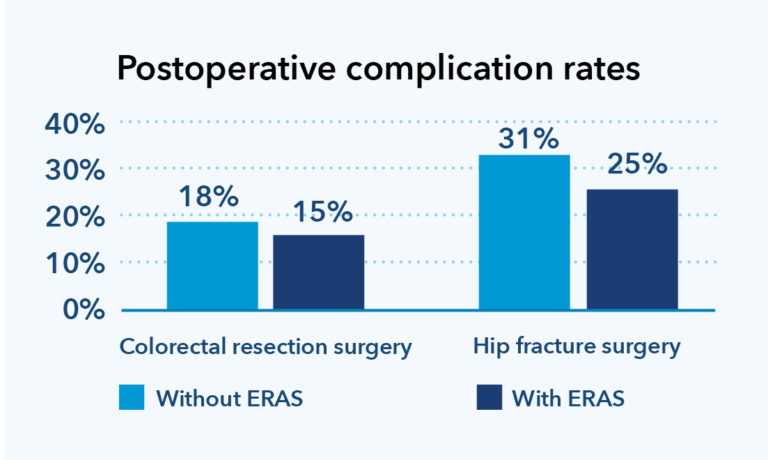
Once implemented, the ERAS protocol decreased opioid prescribing rates by 21%, and early mobility — which helps prevent blood clotting and pneumonia — increased 34% for colorectal patients and 18% for hip fracture patients.5 The new ERAS approach decreased postoperative complications among both colorectal resection and hip fracture surgery patients (see chart). Components of the program have been incorporated into Kaiser Permanente protocols for the majority of surgeries performed today. As a result of these efforts, Kaiser Permanente was selected for the National Committee for Quality Assurance Delivery System Design award in 2019, for work that improves quality and value.6
How Kaiser Permanente’s integrated care and coverage model supported this innovation
High-quality care with clinical decisions made by physicians and patients
Physicians champion quality improvement, ensuring that our care teams practice medicine based on the best, most up-to-date information, incorporating innovative approaches.
Kaiser Permanente clinical leaders decided to undertake a large-scale effort to reduce surgical complications, reviewing the existing literature and working with team members to design an approach that could be rigorously tested and evaluated.
Research and quality improvement
We analyze care management processes and outcomes and use the results to continuously improve. We then share findings from this practice-based clinical research to benefit others beyond Kaiser Permanente. In addition, our care teams can access a constantly updated clinical library, helping us stay abreast of additional new evidence-based approaches.
The care team tested the ERAS program in a few locations to analyze patient outcomes and hone the approach. When the team achieved promising results and began scaling the program, researchers had enough data to understand subtle variations in procedures and results among a diverse set of patients — assessing care patterns and outcomes for more than 15,000 patients. When the ERAS program achieved promising outcomes, the leadership team worked with thousands of staff and scaled the intervention across 20 medical centers in a single year.
Connected, coordinated care teams
Members benefit from well-coordinated care at Kaiser Permanente. Clinicians can easily coordinate with one another and seamlessly refer patients to other team members: primary care physicians, specialists, lab technicians, pharmacists, and other health care professionals.
A single surgery can involve up to 40 staff members, including nurses, physicians, pharmacists, physical therapists, nutritionists, patient care coordinators, health educators, and various subspecialists. Kaiser Permanente’s ERAS clinical pathways provide a timeline and standard set of surgical practices for each team member to follow, helping them coordinate with each other as patients move through preoperative planning, surgery, and recovery.
Aligned planning and budgeting
Across the health plan, the medical groups, and the hospitals, leaders work together as they develop budgets for services and facilities. This promotes attention to quality improvement and operating efficiencies. Resource stewardship is seen as everyone’s responsibility.
Premium dollars should be spent in ways that maximize health value, with a focus on care, interventions, and activities that lead to better health outcomes.
Implementing the ERAS program required close coordination across the health plan, the medical groups, and the hospitals, jointly investing in new infrastructure that could reduce complications, improve the health of our members, and reduce costs.
Kaiser Permanente’s integrated care and coverage model differs from much of the United States health care system, which relies on disconnected clinical practices paid through fee-for-service. These disconnected approaches typically result in highly fragmented care, a focus on quantity of services rather than high-quality care, and an emphasis on acute care rather than long-term investments in population and community health.
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The Kaiser Permanente Northern California Enhanced Recovery After Surgery Program: Design, Development, and Implementation
In this report, we describe the design, development, and implementation of an Enhanced Recovery After Surgery program in the Kaiser Permanente Northern California integrated health care delivery system.
Enhanced Recovery After Surgery Program Implementation in 2 Surgical Populations in an Integrated Health Care Delivery System
A JAMA Surgery study: To evaluate the outcomes of an enhanced recovery after surgery ERAS program among 2 target populations: patients undergoing elective colorectal resection and patients undergoing emergency hip fracture repair.
- V.X. Liu, et al. “The Kaiser Permanente Northern California Enhanced Recovery After Surgery Program: Design, Development, and Implementation.” The Permanente Journal, 21, 17-003, Summer 2017. https://doi.org/10.7812/TPP/17-003.
- Marco Taurchini, Carlo Del Naja, Antonio Tancredi. “Enhanced Recovery After Surgery.” Journal of Visualized Surgery, 4:40, 2018.
- Kaiser Permanente Division of Research, “Enhanced Recovery After Surgery Program at Kaiser Permanente Significantly Improves Surgical Outcomes,” Kaiser Permanente, May 10, 2017, https://spotlight.kaiserpermanente.org/enhanced-recovery-after-surgery-program-at-kaiser-permanente-significantly-improves-surgical-outcomes/.
- V.X. Liu, et al. “The Kaiser Permanente Northern California Enhanced Recovery After Surgery Program: Design, Development, and Implementation.” The Permanente Journal, 21, 17-003, Summer 2017. https://doi.org/10.7812/TPP/17-003, and Kaiser Permanente Division of Research, “Enhanced Recovery After Surgery Program at Kaiser Permanente Significantly Improves Surgical Outcomes,” Kaiser Permanente, May 10, 2017, https://spotlight.kaiserpermanente.org/enhanced-recovery-after-surgery-program-at-kaiser-permanente-significantly-improves-surgical-outcomes/.
- V.X. Liu, et al. “Enhanced Recovery After Surgery Program Implementation in 2 Surgical Populations in an Integrated Health Care Delivery System.” JAMA Surgery, July 19, 2017; doi:10.1001/jamasurg.2017.1032.
- Permanente Medicine, “Region Recognized for Surgical Care Innovations,” October 17, 2019, https://permanente.org/region-recognized-for-surgical-care-innovations/.