
Integrated Care Stories
Pain management and the opioid epidemic
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The challenge
One out of every 5 people living in the United States suffers from chronic pain, and pain management is an important part of clinical care.1 Opioids are often prescribed to people suffering from pain to alleviate their symptoms, but they are highly addictive. Opioid overdoses kill approximately 200 Americans every day.2
The current opioid epidemic started in the mid-1980s, when some studies claimed that opioid pain relievers could be safely prescribed for long-term use. The national opioid prescription rate began to rise in the late 1990s, as members of the medical community became increasingly concerned about undertreatment of chronic pain,3 and as new formulations of opioid drugs were developed and aggressively marketed to physicians and patients. Patient advocates were highlighting the need for better pain identification and treatment, and pain medicine associations began promoting the new opioid formulations as an acceptable chronic pain management approach. Related to these trends, sales of prescription opioids increased dramatically over the next decade.4
Research later found that too many opioids were being prescribed, at dosages that were often too high. This contributed to increases in overuse, overdoses, and deaths. Between 1999 and 2019, deaths from prescription opioid overdoses quadrupled.5 In 2011, the Centers for Disease Control and Prevention declared that overdoses from prescription opioids had reached epidemic levels, the Office of National Drug Control Policy released a call to action, and states began passing guidelines and limits on opioid prescribing.6
The integrated care and coverage solution
At Kaiser Permanente, our integrated care model helped us recognize and respond to the problem. More than a decade ago, through our electronic pharmacy information systems, we identified a notable increase in the amount of opioid prescriptions being filled at our pharmacies. This information was shared with physician leaders who assessed the situation and evaluated emerging evidence on opioid effectiveness and challenges.
We collectively took action to ensure Kaiser Permanente physicians and care teams had the most current information on pain management best practices, non-opioid alternatives to manage pain, and ways to prescribe opioids safely and reduce addiction risks. We created multidisciplinary drug utilization teams to help physicians and other care team members effectively and appropriately manage patients’ pain needs. We updated our computer-based prescribing systems to provide opioid-specific safety alerts, suggest preferred and maximum opioid doses, share links to evidence-based guidelines, and show prompts for alternative treatments or medications. We connected Kaiser Permanente opioid experts with care teams to share current information about opioid risks and best practices in pain management. We also educated patients and offered pain management alternatives to reduce the need for opioids. Kaiser Permanente has continued to provide addiction, detox, and care services for members facing opioid challenges.
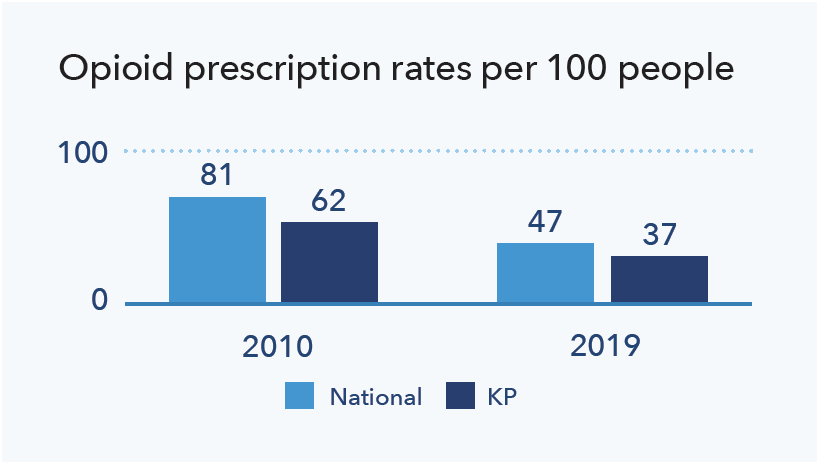
As a result of these actions, Kaiser Permanente reduced its volume of opioid prescriptions earlier than the average nationwide.7 Kaiser Permanente continues to look for new and innovative ways to reduce addiction and prevent overdoses, while providing necessary pain management support.
How Kaiser Permanente’s integrated care and coverage model supported this innovation
High-quality care, with clinical decisions made by doctors and patients
Physicians work with their patients to develop personalized care plans, making decisions about medical care together. To inform those decisions, doctors use the best available evidence and champion quality improvement, ensuring that our care teams practice medicine based on the best, most up-to-date information, incorporating innovative approaches.
The medical field’s understanding of opioid use for chronic pain has shifted over time. As new evidence emerged about addiction risks, physicians needed up-to-date information to make good clinical decisions. At Kaiser Permanente, physicians led efforts to educate and raise awareness among their fellow physicians and other care team members about the emerging evidence, to help them manage patients’ pain appropriately and effectively.
Physicians work closely with each patient to develop personalized care plans informed by current research and best practices. Patients have access to both in-person and online pain management resources, and often can manage pain using non-opioid drugs or through approaches like cognitive behavioral therapy, group pain management classes, mindfulness training, tai chi, acupuncture, or physical therapy. Pain management alternatives can even be used after surgeries, as highlighted in our Enhanced Recovery After Surgery story. When patients need opioids, physicians and patients complete opioid medication agreements after discussing medication use, benefits, risks, alternatives, and expectations, and patients regularly meet with their care team to jointly assess progress and discuss opportunities to reduce risks.
Connected, coordinated care teams
Members benefit from well-coordinated care at Kaiser Permanente. Clinicians can easily coordinate with one another and seamlessly refer patients to other team members — primary care doctors, specialists, lab technicians, pharmacists, and other health care professionals.
A highly coordinated model of care benefits our members. Physicians and care teams from our primary and specialty care, pain management, and addiction medicine departments work closely with each other, and with our pharmacists, to provide effective pain relief without putting our members at risk for opioid-related complications. Care team members throughout our organization have access to current information on pain management best practices.
When needed, Kaiser Permanente members can access support in multiple ways, whether through self-referral, a referral from a primary care doctor or specialist, or through emergency psychiatric services or the emergency department. Patients have wrap-around support, which reduces the risk that people will give up seeking care or will relapse. Depending on their specific needs, patients can access medical detox services, attend one-on-one counseling sessions, access educational classes, attend group therapy sessions, or take part in family education and counseling.
Information-sharing across clinical care teams
Clinicians have access to all Kaiser Permanente medical data for every member they support, enabling care teams to identify opportunities to improve the safety and quality of care. Kaiser Permanente tracks and maintains records over decades, enabling a long-term perspective on each individual’s health over time. Care teams can make well-informed decisions based on a full range of patient information and can easily connect with each other to work effectively as a team.
Care team members can see their patients’ prescribed medications, even if they are being prescribed by different physicians within Kaiser Permanente. This reduces the risk of accidentally overprescribing opioids to a patient. In addition, our computer-based prescribing system provides a centralized mechanism for sharing helpful information with physicians to support them in their patient care and prescription drug decision-making. For patients who need to be on higher doses of opioids for clinical reasons, physicians can prescribe naloxone, a medication that can quickly reverse overdoses.
After early successes at improving overall pain management supports for our clinical care teams and patients in a few of our regions, we implemented the approach quickly across all Kaiser Permanente markets.
Research and quality improvement
We analyze care management processes and outcomes and use the results to continuously improve. We then share findings from this practice-based clinical research to benefit others beyond Kaiser Permanente. In addition, our care teams can access a constantly updated clinical library, helping us stay abreast of additional new evidence-based approaches.
Kaiser Permanente’s investments, as an integrated care organization, in both pharmacy information systems and electronic health record systems allow us to monitor health outcomes and trends. As challenges are recognized, physicians and pharmacists can collectively discuss problems and identify ways to address them together, sharing information quickly across our full network of care team members.
To continue improving care quality, research teams investigate opportunities to better manage pain and reduce addiction. For example, a recent study by Kaiser Permanente researchers found a significant increased risk of opioid overdose among patients who were also taking benzodiazepines and other sedative drugs, highlighting an opportunity to reduce patient risks.8
Individual patients are best served when they have effective pain management support at the lowest possible risk, and communities are safer when we decrease the total quantity of opioids being used. We have shared information about our approach to pain management and opioids and our recommendations with the Centers for Disease Control and Prevention, the Food and Drug Administration, state attorneys general, and other leaders across the country, and helped shape new CDC guidelines on opioids.
Kaiser Permanente’s integrated care and coverage model differs from much of the United States health care system, which relies on disconnected clinical practices paid through fee-for-service. These disconnected approaches typically result in highly fragmented care, a focus on quantity of services rather than high-quality care, and an emphasis on acute care rather than long-term investments in population and community health.
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
Kaiser Permanente’s approach to pain management.
- Zelaya, C., Dahlhammer, J., Lucas, J., and Connor E. “Chronic Pain and High-Impact Chronic Pain Among U.S. Adults, 2019.” National Center for Health Statistics Data Brief No. 390, November 2020, https://www.cdc.gov/nchs/products/databriefs/db390.htm; and Awsare, S., Havens, C., and Lippi, J. “Facing the Opioid Crisis: Practical, Effective Actions We Can Take.” Gastroenterology, May 2019; 156(6) https://pubmed.ncbi.nlm.nih.gov/30682346/.
- Drug Overdose Deaths. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/deaths/index.html. (70,630 drug overdose deaths in a year / 365 days)
- Dupont, S., Bezaitis, A., and Ross, M. “Stemming the Tide of Prescription Opioid Overuse, Misuse, and Abuse.” Health Affairs Forefront. September 22, 2015, https://www.healthaffairs.org/do/10.1377/forefront.20150922.050693/full/.
- Philips, J.K., Ford, M.A., Bonnie, R.J. “Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Washington, DC: National Academies Press, July 13, 2017, https://www.ncbi.nlm.nih.gov/books/NBK458660/.
- Centers for Disease Control and Prevention. (2020, December 07). U.S. Opioid Dispensing Rate Maps. Retrieved from https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html; Centers for Disease Control and Prevention Drug Overdose Overview https://www.cdc.gov/drugoverdose/deaths/prescription/overview.html; and J.K. Philips, M.A. Ford, and R.J. Bonnie. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division. National Academies Press, July 13, 2017, https://www.ncbi.nlm.nih.gov/books/NBK458660/; National Institute on Drug Abuse. Overdose Death Rates. https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates.
- Centers for Disease Control and Prevention. (2011, November 1). Prescription painkiller overdoses at epidemic levels [Press Release]. Retrieved from https://www.cdc.gov/media/releases/2011/p1101_flu_pain_killer_overdose.html; Office of National Drug Control Policy, Epidemic: Responding to America’s Prescription Drug Abuse Crisis, 2011, http://publications.iowa.gov/12965/1/NationalRxAbusePlan2011.pdf; Lee, B., Zhao, W., Yang, K., Ahn, Y., & Perry B. L. (2021, February 12). Systematic Evaluation of State Policy Interventions Targeting the US Opioid Epidemic, 2007-2018. JAMA Netw Open. 2021;4(2):e2036687. doi:10.1001/jamanetworkopen.2020.36687; National Conference of State Legislatures. (2019, June 30). Prescribing Policies: States Confront Opioid Overdose Epidemic. https://www.ncsl.org/research/health/prescribing-policies-states-confront-opioid-overdose-epidemic.aspx; Lee, B., Zhao, W., Yang, K., Ahn, Y., & Perry B. L. (2021, February 12). Systematic Evaluation of State Policy Interventions Targeting the US Opioid Epidemic, 2007-2018. JAMA Netw Open. 2021;4(2):e2036687. doi:10.1001/jamanetworkopen.2020.36687
- Kaiser Permanente internal data (analysis provided by Elizabeth Bentley and Andrew Vidaurreta based on data from Kaiser Permanente National Pharmacy Analytics), and Centers for Disease Control and Prevention. (2020, December 07). U.S. Opioid Dispensing Rate Maps. Retrieved from https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html
- Cho, J., Spence, M., Niu, F., Hui, R., Gray, P., and Steinberg, S. “Risk of Overdose with Exposure to Prescription Opioids, Benzodiazepines, and Non-Benzodiadepine Sedative-Hypnotics in Adults: a Retrospective Cohort Study.” Journal of General Internal Medicine. March 2020; 35(3), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7080944/.